|
Quite obviously, similar to most spinal anaesthetic practices. This aims to provide a aide-memoire for out of hour (and in-hour!) practices where variability in all practitioners can exist. This is only ONE guide to providing a spinal anaesthetic and obviously is not made to replace AAGBI or OAA guidelines. It is something all staff can use to remind themselves of the equipment required and order things are done in. The BNF should always be used when prescribing medication and your patient may not be suitable for NSAID's or opioids OR stipulated antibiotic regimes due to contraindication or allergies. The post-operative analgesic regime is likely to vary a lot between hospitals depending on your local practices.
Furthermore, this does not replace the need for preparation for a general anaesthetic. You should always be mentally and procedurally prepared that the patient is going to have to emergently go to sleep for delivery. The key aim of this document is to provide a snap-shot of information to aid staff help the anaesthetic team in siting a spinal in the safest, quickest way possible in a time-pressured situation. It can be used by everyone to raise the question of whether something on this list is needed, or has been purposefully omitted. Anaesthetic assistants and midwifery staff should be sensitive to the needs to the anaesthetist and the procedure, as, the baby cannot come out via c-section until the spinal is in and working. With everyone working together, this can be achieved more quickly. It allows the questions to be asked such as, "Do you want the oxytocin infusion prepared?" well before the baby comes out, because you have consulted the list of often-needed medications and it has reminded you. It also prompts early discussion with the obstetric team. Perhaps it is not a useful infogram for seasoned practitioners, but it is certainly useful for the junior team seeking to be as thorough as possible.
4 Comments
Melatonin - considered by some to be a 'herbal myth' and others as a useful adjunct to help sleep in ICU patient and adults >55 years old. There is biological plausibility that melatonin could be a useful adjunct to aid restful and efficient sleep in those who could be deplete in melatonin.
Overall - a meta-analysis here in 2013 showed that there was some evidence to say that it could work in some cohorts. Given its relatively safe profile, it could be useful to trial in patients with a sleep disorder. Particularly it could be of use in ICU, but, the evidence is currently out - awaiting a larger RCT. It's a cheap drug and even cheaper in the USA where it is available OTC. In patients who are restless or unable to sleep in a busy ICU, perhaps it has a role in being a first drug of choice before considering more 'heavy' sedative alternatives given it is a non-narcotic. The studies mentioned below are indeed rather small and a few are single-centre analyses, so we cannot say for certain whether there is true efficacy, but many practitioners would agree, it's certainly worth a go providing there are no obvious contraindications in your local formulary (primarily, not to use in patients with autoimmune conditions) and the person does not require heavy sedation for other reasons. Outside ICU, the drug is quite popular with GP's and could even be used more frequently as a first line alternative to Z-drugs or benzodiazepines in a hospital cohort. Sleep deprivation, it will come as no surprise, is rife in hospitals - I think we can all agree, that any adjunct to promote restful sleep without being profoundly 'sedating' could be a useful drug. I look forward to seeing more definitive studies in the future.
Dr. Sergey Motov (USA Emergency Medicine) & Dr. David Lyness (UK/IRE Anaesthetics)
Originally put on this website in July 2016 Taken from Dr Motov's work on a CERTA regime. This is published in conjunction with the CERTA concept explanation here. We can all provide superior analgesia by using medication and techniques other than just opioid medications. This is NOT a definitive list and in all cases, local policies and protocols should be followed. Check your local formularies. This is NOT a prescribing guideline - it is for information ONLY. We do not dispute the role of opioids in many spheres of practice, including emergency medicine, ICU and anaesthetics, rather we wish to highlight the pandemic of high opioid and opiate use. There are many medications available to reduce the amount of opioids used. You may find, when considering your analgesia regimes that opioids are not always the best options for emergency pain issues. We would advocate the use of nerve blocks in the first instance to control acute pain, when feasible.
With respect to alternatives listed for non-radicular back pain, it has been brought to our attention that a new study was presented in 2017 which showed that "diazepam has no benefit when added to naproxen vs placebo" in acute low back pain. See here. This document is for review in 2018 - so please contact us if you have anything to add!
FULLSCREEN
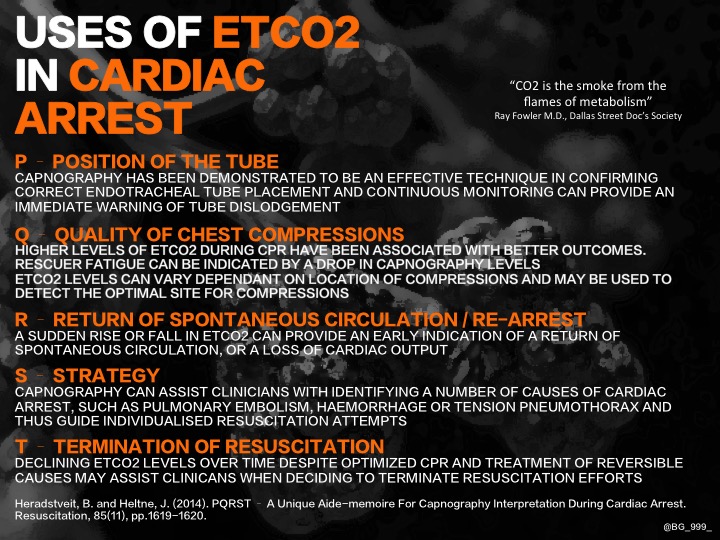
References in document below... Brad Gander in another great infographic, explores the uses of ETCO2 in cardiac arrest, using PQRST!
This was made as an A4 PDF sized infogram which can be downloaded below.
If the graphic is taking too long to view, it can also be seen below as a PDF.
Here is NAP4's example of an emergency intubation checklist.
FULLSCREEN
NB: This is not intended to supersede any guidelines your department may already have in use. All departments facilitating the emergency intubation of patients should have a checklist available.
FULLSCREEN
25/4/16- Real Time Peer Review = 'Nitrous Oxide' was changed to 'Nitric Oxide' WRT vasodilation. Thanks to @pccm_doc
Graphic for the crichothyroidotomy at the bottom of the infogram is from: Scott Clarke - many thanks!
This algorithm is for adult use.
Here is an English NHS's guideline on Tapentadol use.
The cost of Tapentadol in the NHS at present is £37.37 for 58 tablets of 50mg (Tramadol is £2.40 for 58 tablets) |
USE OF THIS WEBSITE IS SUBJECT TO AGREEING TO THIS DISCLAIMER
|
||||||

Free to access Propofology Infograms, eBooks and selected YouTube videos by Dr. David Lyness are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Please attribute all works: 'Based on a work by Dr. David Lyness' at www.propofology.com/resources.
|
Home
About Contact |
ALL SITE USERS SHOULD READ AND AGREE TO THE DISCLAIMER HERE.
Contact via Twitter |
 RSS Feed
RSS Feed