|
Quite obviously, similar to most spinal anaesthetic practices. This aims to provide a aide-memoire for out of hour (and in-hour!) practices where variability in all practitioners can exist. This is only ONE guide to providing a spinal anaesthetic and obviously is not made to replace AAGBI or OAA guidelines. It is something all staff can use to remind themselves of the equipment required and order things are done in. The BNF should always be used when prescribing medication and your patient may not be suitable for NSAID's or opioids OR stipulated antibiotic regimes due to contraindication or allergies. The post-operative analgesic regime is likely to vary a lot between hospitals depending on your local practices.
Furthermore, this does not replace the need for preparation for a general anaesthetic. You should always be mentally and procedurally prepared that the patient is going to have to emergently go to sleep for delivery. The key aim of this document is to provide a snap-shot of information to aid staff help the anaesthetic team in siting a spinal in the safest, quickest way possible in a time-pressured situation. It can be used by everyone to raise the question of whether something on this list is needed, or has been purposefully omitted. Anaesthetic assistants and midwifery staff should be sensitive to the needs to the anaesthetist and the procedure, as, the baby cannot come out via c-section until the spinal is in and working. With everyone working together, this can be achieved more quickly. It allows the questions to be asked such as, "Do you want the oxytocin infusion prepared?" well before the baby comes out, because you have consulted the list of often-needed medications and it has reminded you. It also prompts early discussion with the obstetric team. Perhaps it is not a useful infogram for seasoned practitioners, but it is certainly useful for the junior team seeking to be as thorough as possible.
4 Comments
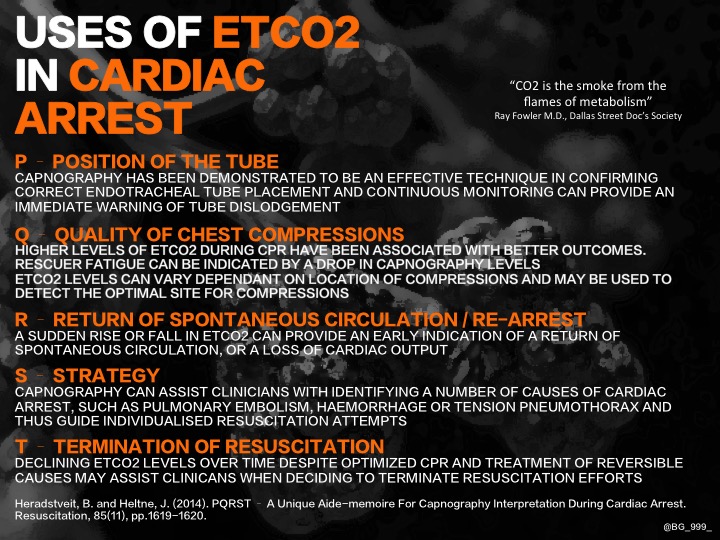
Brad Gander in another great infographic, explores the uses of ETCO2 in cardiac arrest, using PQRST!
This was made as an A4 PDF sized infogram which can be downloaded below.
If the graphic is taking too long to view, it can also be seen below as a PDF.
Here is NAP4's example of an emergency intubation checklist.
FULLSCREEN
NB: This is not intended to supersede any guidelines your department may already have in use. All departments facilitating the emergency intubation of patients should have a checklist available. |
USE OF THIS WEBSITE IS SUBJECT TO AGREEING TO THIS DISCLAIMER
|
||||||

Free to access Propofology Infograms, eBooks and selected YouTube videos by Dr. David Lyness are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Please attribute all works: 'Based on a work by Dr. David Lyness' at www.propofology.com/resources.
|
Home
About Contact |
ALL SITE USERS SHOULD READ AND AGREE TO THE DISCLAIMER HERE.
Contact via Twitter |
 RSS Feed
RSS Feed