|
Quite obviously, similar to most spinal anaesthetic practices. This aims to provide a aide-memoire for out of hour (and in-hour!) practices where variability in all practitioners can exist. This is only ONE guide to providing a spinal anaesthetic and obviously is not made to replace AAGBI or OAA guidelines. It is something all staff can use to remind themselves of the equipment required and order things are done in. The BNF should always be used when prescribing medication and your patient may not be suitable for NSAID's or opioids OR stipulated antibiotic regimes due to contraindication or allergies. The post-operative analgesic regime is likely to vary a lot between hospitals depending on your local practices.
Furthermore, this does not replace the need for preparation for a general anaesthetic. You should always be mentally and procedurally prepared that the patient is going to have to emergently go to sleep for delivery. The key aim of this document is to provide a snap-shot of information to aid staff help the anaesthetic team in siting a spinal in the safest, quickest way possible in a time-pressured situation. It can be used by everyone to raise the question of whether something on this list is needed, or has been purposefully omitted. Anaesthetic assistants and midwifery staff should be sensitive to the needs to the anaesthetist and the procedure, as, the baby cannot come out via c-section until the spinal is in and working. With everyone working together, this can be achieved more quickly. It allows the questions to be asked such as, "Do you want the oxytocin infusion prepared?" well before the baby comes out, because you have consulted the list of often-needed medications and it has reminded you. It also prompts early discussion with the obstetric team. Perhaps it is not a useful infogram for seasoned practitioners, but it is certainly useful for the junior team seeking to be as thorough as possible.
4 Comments
Click HERE to see full infogram
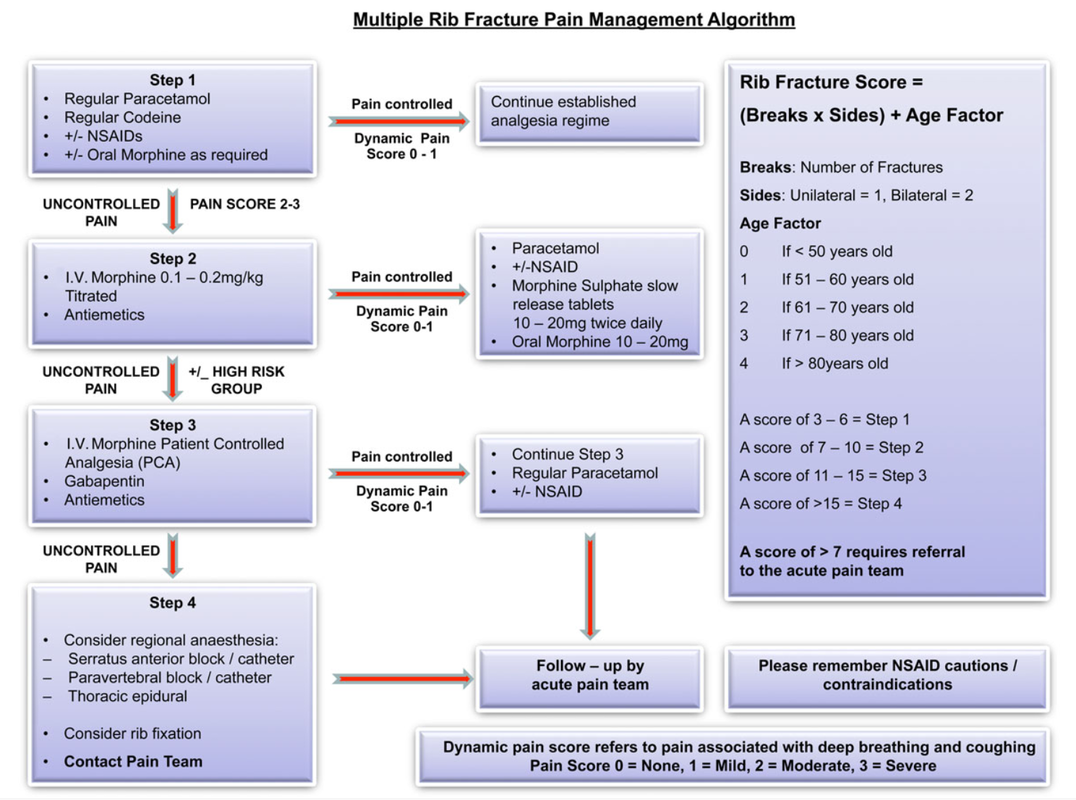
The above algorithm is taken from the BJA Education article, here.
NB: Regional techniques offer high levels of non-narcotising pain relief, such as intercostal blocks and s.anterior blocks +- catheters. (You will all know I am an advocate of the CERTA concept of pain relief, with non-opioids and RA techniques used whenever possible). With all the best will in the world, it is hard to find a trained individual to site or perform such regional techniques in an acute setting 24/7 and in a timely fashion, let alone have a service on the ward that is happy to look after different pumps/complications/troubleshooting etc. This is why this guide will focus on pharmacological management +- Thoracic Epidural where indicated/available. It is also worth noting that non-catheter blocks wear off at various rates depending on local analgesia used, so you still need to be aware of pharmacological management and the step-wise pain pathways. Should 24/7, quick-access Regional Anaesthesia be available in your hospital; this is a great asset and should be used in conjunction with your own local policies.
Rib fractures can be difficult to manage with respect to adequate pain relief and maximised chest safety. There is a high risk, in more complex fractures, of pneumothorax, haemopneumothorax, flail chest and great vessel injury. One of the most significant problems to prevent, (after PTX etc) is the acquisition of an atelectasis induced chest infection, particularly in those with concomitant chest disease and advancing age. You must be able to rapidly and safely control pain levels. We also know that a lot of patients can be managed on the ward with good nursing, physiotherapy and analgesia and that many are not admitted to ICU. It is worth noting that an HDU/ICU admission may be required if pain is not controlled and breathing becomes an issue - you should involve the pain and ICU teams early, but this should not substitute or preclude the admitting team & ED actively trying to control pain using the algorithm above. It will be useful to the acute pain teams to see which, if any, analgesia worked. All patients with rib fractures may not be admitted, but those who are sore enough to should have basic care (mentioned in the infograph) commenced IMMEDIATELY in A&E. Good regimes of escalating pain regimes must be in place from A&E and admission teams and NOT just wait for a pain team review, which can be after a busy weekend or the next working day. It may be nice to allow all patients to have a thoracic epidural sited, but this is not pragmatic in a busy NHS hospital; it will often be the next day or 'after the weekend'. They are also not required for every rib fracture patient. NEVERTHELESS, thoracic epidurals DO have benefit for those who have complex disease processes, fractures and advancing age. They probably should not be inserted due to inadequate attempts to control pain with more conventional pharmacological methods in most patient groups. Surgical wards are used to dealing with PCA's so they often become the first stop of acute pain management. Wards are often not set up to facilitate IV lignocaine/ketamine infusions; if your wards are - you should contact your local pain team to see whether these interventions might be utilised in your place of ward in lieu of a morphine PCA. Do not forget to write up emergency naloxone if using opioids alongside an anti-emetic regime. Here is the best BJA Education Article for scoring rib fractures with advice on pharmacy etc. A final note on pharmacy; PLEASE check the BNF for contraindications of medications in your patient. Renal function is also important with respect to opioids, NSAIDs and Gabapentin etc.
Kudos to David Halliwell - Paramedic who spoke at SMACC DUB in 2016, delivering this wonderful topic
Resus.org.uk has all the latest guidelines on Cardiac Arrest and Advanced Life Support You can watch (free) David Halliwell's amazing SMACC Talk here. He talks about 'sneaky helpful ventilations' - so beware of over ventilating the patient in cardiac arrest!
Afterword
by Dr. David Lyness & Mark Dornan Lack of sleep is a major problem in hospitals across the world. Hospitals are NOT quiet places; we all know this. Working together we can help patients get better sleep in order that they might have better outcomes, better hospital experiences, more energy and less complications during their stay. I would have to say, I am a massive advocate of the eye masks and ear plugs. They are cheap, simple interventions that can be supplied by the ward or bought by patients for a nominal fee. Wholesale, these can be bough for pence and likely reduce vastly more costly complications associated with sleep deprivation. The caveat being, they can really only be used by patients who are well enough to take them off (this is common sense). It's also a strange practice to give patients caffeinated drinks before bed-time. Coffee & Tea are both caffeinated and stimulate an awake state. Decaf options should be available for the patients who 'cannot cope' without a bed-time cuppa! Fruit-like 'herbal' teas should also be brought in by patients or supplied by the ward. It is furthermore an even stranger practice to give people caffeinated drinks along with their insomnia medications like zopiclone etc. Red Bull and other highly caffeinated drinks such as coke, lucozade and sports drinks really should be limited too. Mark also raises the excellent point of caffeinated drinks and continence in the elderly. Caffeine drinks further disturb sleep by increasing the production of urine and therefore frequency of micturition - waking patients up to urinate further deteriorates sleep quality. Considerate nursing and medical practice is key to helping patients sleep well. Share your thoughts on twitter @gas_craic :-) |
USE OF THIS WEBSITE IS SUBJECT TO AGREEING TO THIS DISCLAIMER
|

Free to access Propofology Infograms, eBooks and selected YouTube videos by Dr. David Lyness are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Please attribute all works: 'Based on a work by Dr. David Lyness' at www.propofology.com/resources.
|
Home
About Contact |
ALL SITE USERS SHOULD READ AND AGREE TO THE DISCLAIMER HERE.
Contact via Twitter |
 RSS Feed
RSS Feed