|
And so the trend of monthly and annual summaries continues!
Here are some of the more memorable trials from February 2018 from ICU land. Hard to be completionist, or fit everything in one A4 page, but plenty of food for thought and continued discussion! Enjoy (Full Screen Here) (PDF Download)
0 Comments
Below is an educational resource about how to begin to interpret ABG's and what the components seen on them mean in real-terms.
As always - not a clinical guideline, just a learning resource. All lists are not exhaustive. Note that many pathologies can cause a respiratory alkalosis via hyperventilation. If you would like to print it out to use in a department, or as a teaching handout, please either let me know on Twitter, or email me at [email protected] - so I can keep a portfolio record. PDF here. *please note you can also use the mnemonic CAT-MUDPILES for the high anion gap causes - see here.
This is a four-page document outlining key considerations in the history taking, investigation and management of critically ill patients surrounding the time of discussion with the HDU/ICU team.
THIS IS A WORK IN PROGRESS - FEEL FREE TO CONTACT AND CONTRIBUTE! 1. It's a teaching & learning tool, rather than a document where people actually sit down and fill it in 2. It is intended to provide a structure/framework for thought processes around referrals to HDU/ICU
RATIONALES
WHAT THIS IS RESOURCE IS NOT These documents are NOT guidelines or policies and have not been ratified/tested for clinical use. These documents do not replace the need for: Seeking help immediately, if required Clinical judgement and assessment Discussing patient's with the patient's consultant (on-call) 'Referral algorithms' are a tricky business - which is why, this is not one - it's a learning resource, and not a clinical guideline or mandate. Documents and checklists should not prevent you from seeking skilled help early. The documents do suggest things you should be mindful of, in sick patients. It is impossible to predict every eventuality - but many of these principles are ubiquitous to all referrals. With thanks given to Dr. Jonny Wilkinson, Dr. Adrian Wong and Dr Segun Olusanya for their thoughts on this project, as well as to everyone who has already commented on Twitter.
Hover over the infograph below and you will see four slides of content you can peruse through.
PDF Download Available here.
Some interesting trials are promised in 2018.
Here are some of the more interesting ones (mostly SR's) that sprang up over January 2018... As always, these are to provoke discussion on twitter, rather than me or anyone else giving a definitive 'what do I think' on them. Head on over to the websites mentioned at the bottom of the infographic to see some excellent commentaries on other trials. Particularly www.thebottomline.org.uk ADRENAL was launched at Critical Care Reviews in January 2018. The rest that I have featured are systematic reviews. Many thanks to all publishers, authors and researchers who endeavour to make their research free to access to the #FOAMed community. LINKS TO THE STUDIES/SR's ADRENAL GLYCAEMIC CONTROL IN TBI INTUBATION IN THE CRITICALLY ILL PROPOFOL FOR SLEEP IN ADULT ICU PATIENTS CLICK HERE TO SEE THIS FULL-SCREEN  It has certainly been a year of great #FOAMed for Critical Care and Anaesthetics... In this short round-up of the Propofological year - we look at 10 topics of the year as well as projects I've been involved in, infographics we've created, podcasts, YouTube channel, #IFAD2017 and perhaps talk about some of what's to come in 2018. 1. SEPSIS 3.000000 - is still here...! Seems to be at every conference I attend! 2. POCUS - a fan favourite in the community. More people picking up the probe this year! A great deal of excellent resources popping up all over the place. Critical Care Northampton have excellent resources for POCUS-mad practitioners! 3. Fluid Management (less seems to be more?) - #IFAD2017 hammered home the need to REALLY think about fluid prescriptions in the critically ill. They highlighted sepsis is primarily a condition of vasoplegia where patients may also require fluid... it's not solely a problem of hypovolaemia. This probably ties in with our own experiences with IV fluids where there is, in many conditions, a resus phase, plateau and de-resuscitation phase. Such is the scale of the problem we came together and developed a protocol for fluid prescription focusing on the four D's... IV FLUID PROTOCOL 4. Renal Issues - bicarb/NAC protection is a bit of a myth when it comes to IV contrast. We may not have been blown away by the outcome of the PRESERVE trial, but it certainly helped to confirm suspicions. 5. A fascinating sepsis trial in Zambia increase focus onto current sepsis management in developing countries. Not generally applicable to developed countries population, but still enormous amount of food for thought and a lot of interesting data. Many patients were HIV positive, and the inotrope used was dopamine (cheap and widely available). Lots of questions remain to be answered (and asked) about why this protocol performed so badly vs standard care. 6. Presentation skills at conferences still leave a lot to be desired. At nearly every conference, I could imagine Mr Ross Fisher's despairing face, wailing at the presenter for reading out endless slides of boring data. A key piece of advice would be that people do not come for you to read them your data, they come to hear your opinion on your data. Provide articles in advance, provide data in advance and deliver a TALK to your audience. More about P3 presentation skills here by Ross Fisher... 7. Opioid alternative regimes are still interesting a vast number of practitioners out there. I published a list of alternatives with Dr. Sergey Motov in 2016, which vent viral at this year's @Core_EM via Dr. Anand Swaminathan. You can see it here along with the 'concept' here. Perhaps one of the things I would like to mention about this piece of work is that they are SUGGESTIONS for opioid alternatives. We would hate to be labelled as zealots when it comes to an anti-opioid stance - it would be foolish not to recognise the important role of opioids as an analgesic - particularly when I use them in anaesthetics every day! But it would be equally foolish to approach all pain-types with opioids. There is an evidence base that Dr Motov has ploughed into and referenced for this resource, and it does require an update in 2018 (given new evidence about diazepam in back pain etc.) - which will be coming up in January! There is also plenty of room for multi-modal analgesia within many specialties. 8. A little more about #IFAD2017. Many thanks to the wonderful Prof. Manu Malbrain for inviting me to form part of the core faculty at IFAD this year. He is an inspirational man and a phenomenal host, who really understands the power of social media in intensive care medicine. Unapologetic of his technological stance when it comes to a fairly traditional conference, he has revolutionised this event and made more than 24 million impressions via Twitter, world-wide as well as boosting real-term participation of the conference by up to 1000 extra via webinars and online interaction. The material that was curated by the social media team is still being used at this moment by people across Twitter and the internet. I look forward to joining him again for the next event. 9. Born out of the IFAD social media team was a group of us who wanted to move forward together in critical care #FOAMed and develop a new and exciting project which will bring us a new and exciting style of critical care conference in the UK.... more on this in 2018. 10. Discussions ebb and flow in Twitterland, some of them more tiresome that others. A desire to move on from discussions over DL vs VL and Sux vs Roc is growing and hopefully will continue to flourish into 2018. Having spoken about this in some of our podcasts, I think a good proverb may be, for many, many, many aspects of medicine; "There are many ways to skin a cat". Often, it's good to disagree - but - sometimes it's better to just move on and discuss something else... at least for a while. Below are some great resources to highlight some of the efforts that have dominated my own year in educational material: Infographs on Cardiac Arrest, Opioid Alternatives, Rib Fracture Management and IV Fluid Constituents were amongst the popular of 2017 for Propofology followers. You can see a full list of the infograms here. The Propofology/QuickMedic YouTube channel continues to grow with free content. Check out one of our first videos in 2017 here... many more on the channel! The summary that I have made of the top #FOAMed trials for ICU is available in infogram form, here. www.CriticalCareNorthampton.com by Dr. Jonny Wilkinson continues to provide excellent blog posts, trawling the net for excellent critical care articles and projects. We have collaborated extensively this year with #IFAD2017 and in other projects to bring some excellent material to the fore. We hope you have enjoyed this as much as we have. Jonny has my particular thanks this year as being a wonderful contributor to Propofology projects as well as getting us involved in as many different aspects of #FOAMed as practically possible. Check out some of our stuff: IV FLUID PROTOCOL STOP BEFORE YOU BLOCK #IFAD2017 QUOTES & GRAPHICS #ICSSOA2017 QUOTES AND GRAPHICS PODCASTS TheBottomLine from the Wessex Deanery created a brilliant review of their top ten trials from 2017. I collated them in an infographic here, but check them out for yourself! CriticalCareReviews.com has its latest meeting in JANUARY of 2018! Lots of #FOAMed content to come from that. You can see all the old content from 2017 (still extremely relevant) here. Propofology will continue to be a site of resource curation and promote social media in medical education to all levels of practitioners, in all corners of the world. Have a wonderful new year everyone. Be kind to each other. Thanks so much for everyone's support of the Propofological endeavours throughout 2017... there will be many more in 2018.
Here is a compilation of some of the major trials in 2017 for ICU.
You can see many of them in the HOT ARTICLES section of the phenomenal CriticalCareReviews.com You can see many of them reviewed on www.TheBottomLine.org.uk as well as our partner website www.CriticalCareNorthampton.com The references for all of these trials can be found in the various months here or via a quick google search. We encourage you ALL to read the trials and decide for yourself - these are not individual reviews and merely summarise what the authors themselves have stated in their trial. The idea of infographics like this is, that via a quick read, you can identify some good #FOAMed articles that may peak your interest and you can explore them further. They also serve as good reminders to what goes on in a busy academic year. Enjoy! PDF FILES: (Please print out the document without alterations - keeping the websites etc on the page)
I was delighted when TheBottomLine did a best of the best review of their ICU trial summaries this year.
I have collated them below in an infographic. You have to check out their website to have a good look at all of the tremendous work they've done in more detail! CLICK HERE Merry Xmas & Happy New Year!
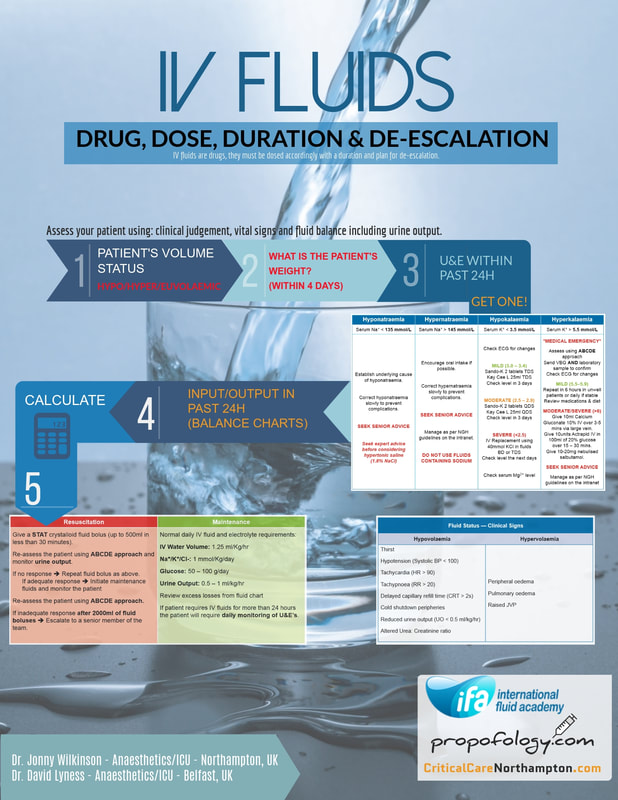
Following on from our previous post on our IV fluid protocol (here). We would LOVE to hear your ideas for it's implantation and development in the coming weeks, months and years.
Have a listen to our Podcast where we discuss how the project came about, the problem with IV Fluid prescribing and our call to action to get a similar idea installed in a trust near you. Even more documents and tables coming soon! Please, if you do want to use our material please attribute it to us so we can show others amazing #FOAMed resources. Also, do let us know! We'd be delighted to hear from you. Don't forget to check out the rest of the Propofology Podcasts here. Check out the updated CriticalCareNorthampton.com blog too!
A joint collaboration from Dr. Jonny Wilkinson and Dr. David Lyness for International Fluid Academy.
Here we present Dr. Wilkinson & Dr Abdul Gomaa's excellent work on establishing a FLUID PROTOCOL for patients, establishing key processes within the prescription and considerations of IV fluids in the hospital. Both of us are attending Internation Fluid Academy in Belgium this year (#IFAD2017) as Faculty. This is a high-end academic conference in Intensive Care Medicine that will have a heavy social media presence - focusing on fluid management, haemodynamics, POCUS and ICU management of the patient in fluid excess. As with ALL FOAMed material, this protocol is for information only and we cannot take any responsibility for its use outside our spheres of practice. Nevertheless, it is enough to give you plenty of food for thought in creating your own flow-sheets in your own hospitals. PS: The image is below, but you can see it in high definition and full-screen using this link here.
Quite obviously, similar to most spinal anaesthetic practices. This aims to provide a aide-memoire for out of hour (and in-hour!) practices where variability in all practitioners can exist. This is only ONE guide to providing a spinal anaesthetic and obviously is not made to replace AAGBI or OAA guidelines. It is something all staff can use to remind themselves of the equipment required and order things are done in. The BNF should always be used when prescribing medication and your patient may not be suitable for NSAID's or opioids OR stipulated antibiotic regimes due to contraindication or allergies. The post-operative analgesic regime is likely to vary a lot between hospitals depending on your local practices.
Furthermore, this does not replace the need for preparation for a general anaesthetic. You should always be mentally and procedurally prepared that the patient is going to have to emergently go to sleep for delivery. The key aim of this document is to provide a snap-shot of information to aid staff help the anaesthetic team in siting a spinal in the safest, quickest way possible in a time-pressured situation. It can be used by everyone to raise the question of whether something on this list is needed, or has been purposefully omitted. Anaesthetic assistants and midwifery staff should be sensitive to the needs to the anaesthetist and the procedure, as, the baby cannot come out via c-section until the spinal is in and working. With everyone working together, this can be achieved more quickly. It allows the questions to be asked such as, "Do you want the oxytocin infusion prepared?" well before the baby comes out, because you have consulted the list of often-needed medications and it has reminded you. It also prompts early discussion with the obstetric team. Perhaps it is not a useful infogram for seasoned practitioners, but it is certainly useful for the junior team seeking to be as thorough as possible.
Click HERE to see full infogram
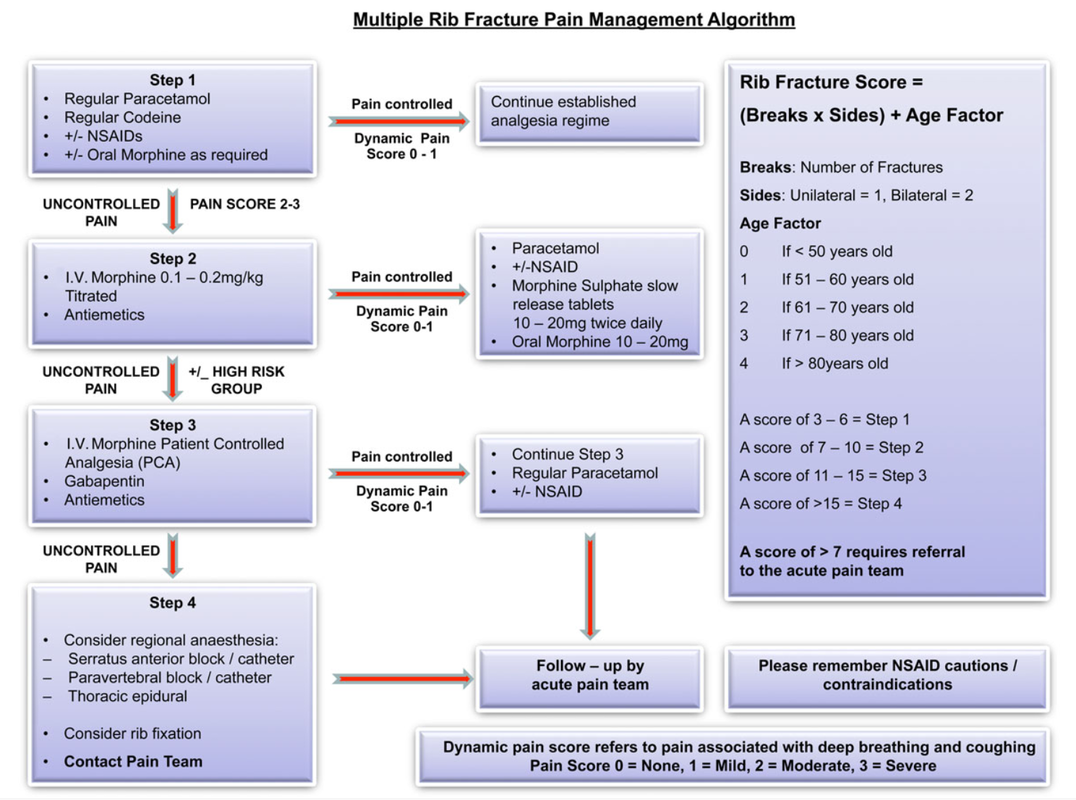
The above algorithm is taken from the BJA Education article, here.
NB: Regional techniques offer high levels of non-narcotising pain relief, such as intercostal blocks and s.anterior blocks +- catheters. (You will all know I am an advocate of the CERTA concept of pain relief, with non-opioids and RA techniques used whenever possible). With all the best will in the world, it is hard to find a trained individual to site or perform such regional techniques in an acute setting 24/7 and in a timely fashion, let alone have a service on the ward that is happy to look after different pumps/complications/troubleshooting etc. This is why this guide will focus on pharmacological management +- Thoracic Epidural where indicated/available. It is also worth noting that non-catheter blocks wear off at various rates depending on local analgesia used, so you still need to be aware of pharmacological management and the step-wise pain pathways. Should 24/7, quick-access Regional Anaesthesia be available in your hospital; this is a great asset and should be used in conjunction with your own local policies.
Rib fractures can be difficult to manage with respect to adequate pain relief and maximised chest safety. There is a high risk, in more complex fractures, of pneumothorax, haemopneumothorax, flail chest and great vessel injury. One of the most significant problems to prevent, (after PTX etc) is the acquisition of an atelectasis induced chest infection, particularly in those with concomitant chest disease and advancing age. You must be able to rapidly and safely control pain levels. We also know that a lot of patients can be managed on the ward with good nursing, physiotherapy and analgesia and that many are not admitted to ICU. It is worth noting that an HDU/ICU admission may be required if pain is not controlled and breathing becomes an issue - you should involve the pain and ICU teams early, but this should not substitute or preclude the admitting team & ED actively trying to control pain using the algorithm above. It will be useful to the acute pain teams to see which, if any, analgesia worked. All patients with rib fractures may not be admitted, but those who are sore enough to should have basic care (mentioned in the infograph) commenced IMMEDIATELY in A&E. Good regimes of escalating pain regimes must be in place from A&E and admission teams and NOT just wait for a pain team review, which can be after a busy weekend or the next working day. It may be nice to allow all patients to have a thoracic epidural sited, but this is not pragmatic in a busy NHS hospital; it will often be the next day or 'after the weekend'. They are also not required for every rib fracture patient. NEVERTHELESS, thoracic epidurals DO have benefit for those who have complex disease processes, fractures and advancing age. They probably should not be inserted due to inadequate attempts to control pain with more conventional pharmacological methods in most patient groups. Surgical wards are used to dealing with PCA's so they often become the first stop of acute pain management. Wards are often not set up to facilitate IV lignocaine/ketamine infusions; if your wards are - you should contact your local pain team to see whether these interventions might be utilised in your place of ward in lieu of a morphine PCA. Do not forget to write up emergency naloxone if using opioids alongside an anti-emetic regime. Here is the best BJA Education Article for scoring rib fractures with advice on pharmacy etc. A final note on pharmacy; PLEASE check the BNF for contraindications of medications in your patient. Renal function is also important with respect to opioids, NSAIDs and Gabapentin etc.
Kudos to David Halliwell - Paramedic who spoke at SMACC DUB in 2016, delivering this wonderful topic
Resus.org.uk has all the latest guidelines on Cardiac Arrest and Advanced Life Support You can watch (free) David Halliwell's amazing SMACC Talk here. He talks about 'sneaky helpful ventilations' - so beware of over ventilating the patient in cardiac arrest!
Afterword
by Dr. David Lyness & Mark Dornan Lack of sleep is a major problem in hospitals across the world. Hospitals are NOT quiet places; we all know this. Working together we can help patients get better sleep in order that they might have better outcomes, better hospital experiences, more energy and less complications during their stay. I would have to say, I am a massive advocate of the eye masks and ear plugs. They are cheap, simple interventions that can be supplied by the ward or bought by patients for a nominal fee. Wholesale, these can be bough for pence and likely reduce vastly more costly complications associated with sleep deprivation. The caveat being, they can really only be used by patients who are well enough to take them off (this is common sense). It's also a strange practice to give patients caffeinated drinks before bed-time. Coffee & Tea are both caffeinated and stimulate an awake state. Decaf options should be available for the patients who 'cannot cope' without a bed-time cuppa! Fruit-like 'herbal' teas should also be brought in by patients or supplied by the ward. It is furthermore an even stranger practice to give people caffeinated drinks along with their insomnia medications like zopiclone etc. Red Bull and other highly caffeinated drinks such as coke, lucozade and sports drinks really should be limited too. Mark also raises the excellent point of caffeinated drinks and continence in the elderly. Caffeine drinks further disturb sleep by increasing the production of urine and therefore frequency of micturition - waking patients up to urinate further deteriorates sleep quality. Considerate nursing and medical practice is key to helping patients sleep well. Share your thoughts on twitter @gas_craic :-)
Above is a 'cheat sheet' or, full data list for the sympathomimetics commonly encountered in medicine, particularly anaesthetics, ICU and emergency medicine. Broadly divided out into alpha, beta, dopamine agonists and phosphodiesterase inhibitors. It is key to understand the actions that each receptor causes; there is often overlap. There is a PDF above for a HD copy of the sheet.
Adapted from a St. George's Hospital London, Anaesthetic Department Poster.
** Clear fluids including water, pulp-free juice and tea or coffee without milk.
FULLSCREEN
There honestly is no such thing as 'fast from midnight' any more. One has FEWER complications, length of stay and hunger issues if you are allowed to drink clear fluids up to 2 hours pre-op. We should be challenging practices from ward-based patients where they are sometimes fasted up to an inch of their life! No-one from the anaesthetic team will mind being spoken to about fasting times.
This is for an elective cohort of patients. This is unlikely to be a suitable mantra for most emergency operations that include a rapid sequence induction. THINK DRINK! References: AAGBI ESAHQ
Existe el concepto errado de que #FOAMed es sólo para personas interesadas en la medicina de Urgencias y Prehospitalario. Es cierto que grran parte del movimiento está dedicado a estas especialidades, pero existe una inmensa variedad de otras especialidades que utilizan #FOAMed para difundir, discutir y desarrollar ideas y mejorar sus competencias.
Esta guía es para todos ustedes, allá afuera, que buscan una pequeña ayuda para descubrir el movimiento #FOAMed. Quizás quieres involucrarte en el ciclo 24/7 de novedades en tu especialidad o quizás quieres contribuir. En el 2016, esto no podría ser más fácil.
Como comenzar 1. Entra a twitter. Crea una cuenta gratuita y usa la etiqueta #FOAMed para descubrir a quien seguir 2. Instala twitter en tu teléfono. Verás las actualizaciones de los que sigues en tu especialidad. 3. Crea una lista (marcadores) de tus blogs o páginas web favoritas que utilizan #FOAMed 4. Googlea #FOAMed y tu especialidad para ver los resultados 5. Usa el sitio LinksMedicus para encontrar las páginas #FOAMed de tu especialidad como también otros sitios increíbles! 6. Involúcrate en conversaciones utilizando en hashtag #FOAMed en twitter 7. Inicia conversaciones acerca de cualquier tema médico utilizando el hashtag #FOAMed junto a #Radiologia, por ejemplo 8. Invita a tus colegas a hacer lo mismo- caras amigas con mucho que aportar. 9. Pon tus presentaciones online utilizado Slideshare o alguno similar, es gratis. Puedes linkearlo a twitter! 10. Si tienes un montón de material o presentaciones, crea un blog gratuito en Wordpress o similares y publícalos online! Aquí hay algunas herramientas de búsqueda #FOAMed
Melatonin - considered by some to be a 'herbal myth' and others as a useful adjunct to help sleep in ICU patient and adults >55 years old. There is biological plausibility that melatonin could be a useful adjunct to aid restful and efficient sleep in those who could be deplete in melatonin.
Overall - a meta-analysis here in 2013 showed that there was some evidence to say that it could work in some cohorts. Given its relatively safe profile, it could be useful to trial in patients with a sleep disorder. Particularly it could be of use in ICU, but, the evidence is currently out - awaiting a larger RCT. It's a cheap drug and even cheaper in the USA where it is available OTC. In patients who are restless or unable to sleep in a busy ICU, perhaps it has a role in being a first drug of choice before considering more 'heavy' sedative alternatives given it is a non-narcotic. The studies mentioned below are indeed rather small and a few are single-centre analyses, so we cannot say for certain whether there is true efficacy, but many practitioners would agree, it's certainly worth a go providing there are no obvious contraindications in your local formulary (primarily, not to use in patients with autoimmune conditions) and the person does not require heavy sedation for other reasons. Outside ICU, the drug is quite popular with GP's and could even be used more frequently as a first line alternative to Z-drugs or benzodiazepines in a hospital cohort. Sleep deprivation, it will come as no surprise, is rife in hospitals - I think we can all agree, that any adjunct to promote restful sleep without being profoundly 'sedating' could be a useful drug. I look forward to seeing more definitive studies in the future. |
USE OF THIS WEBSITE IS SUBJECT TO AGREEING TO THIS DISCLAIMER
|
||||||||||||||||||||||||||||||||||||||

Free to access Propofology Infograms, eBooks and selected YouTube videos by Dr. David Lyness are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Please attribute all works: 'Based on a work by Dr. David Lyness' at www.propofology.com/resources.
|
Home
About Contact |
ALL SITE USERS SHOULD READ AND AGREE TO THE DISCLAIMER HERE.
Contact via Twitter |


 RSS Feed
RSS Feed