|
Foremost, I have to thank the team at ESICM and Dr. Adrian Wong and Joel Alexandre (CEO) for inviting me to cover the event for Social Media and #FOAMed. When I think back to much earlier conferences across Europe and the lack of good social media coverage, it is clear that over the past number of years we have come a very long way! As well as the presentations, ePosters and content being freely available online for #FOAMed use, we now cover conferences on social media in real-time, allowing those across the world to access content that is potentially practice-changing, from the comfort of their own twitter feed. Technology is better, WIFI is stellar and Melia Castilla in Madrid has been an excellent conference centre with lovely amenities and very courteous staff. Pleasantries out of the way, what do I make of the conference so far? ESICM continues to deal with the dichotomy between the scientist and the physician very well by essentially offering content that is suitable for both. Prizing highly academic and scientific content, it essentially separated 'major' content into sections, with Day 1 focusing on physiology and application of such science to clinical practice and day 2 focusing on more clinical conundrums alongside the rudimentary scientific investigations. There has been a focus on mechanical ventilation as well as oesophageal and diaphragmatic muscle movement - with some key messages outlined below. Perhaps a more poorly understood area of our practice is SLEEP in ICU patients, which was dealt with expertly by Dr Demoule of France yesterday. Sleep is profoundly disturbed in ICU with a myriad of clinical and humanitarian (!) consequences for our patients. Many of the slides and take-home messages are included in my trawl of graphics below. Oesophageal pressures have been illuminated to me, as a clinician who has never had the opportunity to use NAVA or an oesophageal pressure probe. Getting to speak to a number of PhD students in technical medicine has shown me its potential use and applications to the patient; again illustrated in some of the slides below. I do think there is still a lot of work to be done in these areas before we can be entirely incorporating of the devices in ICU. It may come a day where they are standard pieces of kit. There were interesting talks on respiratory drive and its relevance to ICU ventilation - and continuing on this theme, how 'strong' spontaneous breathing may not be particularly beneficial for patients on assist.... more on that in Day 2's review. Dead-space monitoring was again a fascinating topic and the industry specialists were showing off their wares in the sponsor's area. It was useful to be able to see the Bohr equation used in real-time! Dr Wong commented how it is unusual to routinely use dead-space monitoring and I would tend to agree. The idea is that it helps with prognosticating in ARDS patients and had a variety of uses in ECMO and permissive hypercapnia - most importantly, it seems to help with PEEP selection and has 'a potential' to monitor lung over-distension. (More info in the slides below). A whirlwind tour though radiological history showed us what we have learned from CT scans with respect to ARDS and none other than Prof Gattinoni discussed the developments since 1986 right up to 2018. It's amazing what we can see of ARDS on a CT scan of the chest as well as uptake scans, showing true perfusion and ventilation. Not a session whereby it was encouraged for all patients to get a CT scan, just rather what they have shown us throughout the years as fidelity has increased (More info in slides below) Lots more to say about Day 1 and lots of info in the slides below - but do continue to follow @Gas_Craic on twitter and #LUNG18 for all the conference pearls, slides and discussions as they unfold. Take care & speak soon!
1 Comment
ESICM Chair of Division MAURIZIO CECCONI writes, "Monitoring is crucial to properly understand and treat our patients with respiratory failure. The vast majority of patients admitted to our ICUs, for any reason, require some form of ventilatory support. The complexity of the patients we treat is increasing and we face challenges every day at the bedside that require complicated and sometimes opposing solutions. In this respect, over the last year, the importance of proper, multifaceted monitoring tools has emerged, not only to minimise the additional injuries, but also to tailor the therapy to individual patients’ needs" To that end, kicking off the conference, will be a talk on what we have learned about ARDS from CT scans. This is not a new concept of course, covered by P STARK from 1987 - but radiology and its basic fidelity have changed radically over the past decades. Already we have seen in 2018, Matthieu JABAUDON from Université Clermont Auvergne unveiling his thoughts on distinct ARDS morphotypes based on lung imaging patterns. It will be fascinating to see what insight the panel are brining to us at LIVES 2018. Looking at the rest of the day tomorrow we are looking at respiratory drive, shunt, gas exchange, controlled ventilation, PEEP, oesophageal and transpulmonary pressures. A welcome update for a lot of us and key components of setting the scene properly for understanding what exactly we can monitor and why it 'might' matter. We're also seeing a real plethora of poster presentations on LOTS of different topics... (see the end of this post) Oesophageal pressures, transpulmonary pressures and diaphragmatic contractility will all be up for discussion at this conference - particularly as ever more inventive ways of monitoring these parameters become commercially available and even incorporated into ventilator modes. The question I will be trying to ask myself and answer is 'do they really matter'? The bio-plausibility of most things discussed at conferences rarely gets frowned upon, but the pragmatics of implementing changes and 'advancing' our monitoring will cost considerable amounts of money and resources. It will be fascinating to see whether there is anything new to glean from the research and whether the speakers can convince us that certain modes are superior or whether they warrant further investigation. I'll try to relay as much of the poster-presentation content as possible- some of the topics really do look fascinating. Don't forget to follow @gas_craic on Twitter and the hashtag #LUNG18 for constant updates from the conference. See the topics of some of those awesome poster/oral presentations below....
We have a REALLY packed schedule in Madrid this year with so many topics and excellent speakers hitting the floors for discussion.
YOU CAN SEE THE ESICM PAGE ON THE EVENT HERE.
Just some of the material we're going to be covering at the event is below as well as a copy of the programme! :-) Lots of talks on monitoring, COPD, diaphragm contractility and its utility in monitoring. All in all, it's shaping up to be a wonderful few days - so I'll catch you on Twitter :-) See the poster below fullscreen here.
For those of you who have been living in a wormhole far in the Delta Quadrant, the fact that The Intensive Care Society's SOA meeting was held this week, may have passed you by.... A great conference that spanned a lot of the nooks and crannies of ICU. This blog article is a 'Too Long Didn't Read'/ TLDR article to give some pertinent one-liners of the conference for those of us who were too busy to get to the conference. A massive shout out to the wonderful Dr. Aoife Abbey or 'Scribbling Dixie' @WhistlingDixie4 for her amazing graphics - see them, and FAR much more besides here. Also to the ever-present Jonny Wilkinson, who of late has become my #FOAMed Partner in Crime... More to come on some of the SOA2017 content - via podcasts and interviews! Twitter can get quite busy, so lets dive into the best picture tweets of the conference. Aoife Abbey's Summary Graphics from Twitter (click)Aoife's brilliant slides illustrate some of the key messages that were flagged up during SOA:
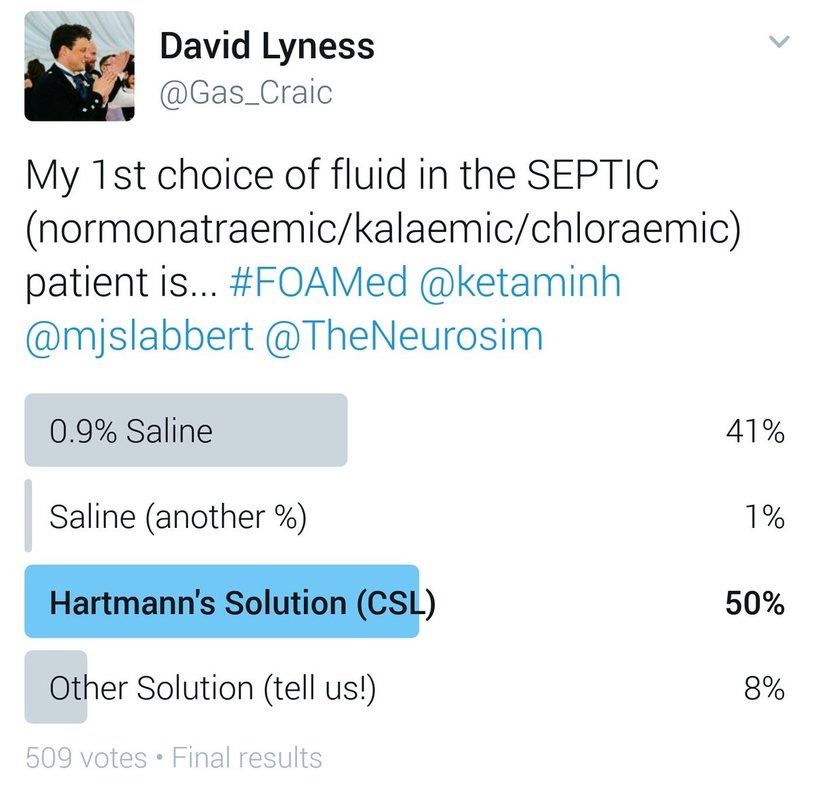
509 #FOAMed users were polled over 24h as to their preference of fluid regime in the septic patient with normal sodium, potassium and chloride levels.
The results are above with CSL coming first, just ahead of NS (0.9%). Obviously nothing particularly robust about the survey, merely an interesting snapshot of users as to their preference. Interesting to note, that much of the 8% who stated another fluid preference, cited Plasmalyte (or similar balanced solutions) as their choice of fluid. The question often gets raised on whether there is a demonstrable difference in outcome between a lot of the balanced crystalloids themselves, or versus NS. There would need to be larger trials performed to ascertain this. Here are some interesting reads on the topic: Avila et al - The Use of Fluids in Sepsis Lavesque et al - Fluid Choice in Sepsis, Does it Matter? Chang et al 2016 - Choice of Fluid Therapy in the Initial Management of Sepsis, Severe Sepsis, and Septic Shock. Click here
Bag mask ventilation is the cornerstone of airway management. It’s often considered a basic procedure, but there is nothing “basic” about BVM ventilation. Skill acquisition requires extensive training and experience. It’s not pretty, sexy, or glamorous. Most people perform it poorly even though it’s an essential part of good airway management. In this tutorial article, ACLS medical go through some great tips and advice on becoming a BVM master. Great work guys! TLDR: Conclusion: - BVM ventilation is a difficult skill for providers at all levels and specialties. - The traditional CE method is not very effective, and sometimes totally ineffective. - Use ETCO2 as an objective measurement. - Adopt the “two thumbs down” technique - Deliver breaths slowly - Only compress 1/3 of the bag - Give breaths quickly during cardiac arrest, but allow full release of BVM |
USE OF THIS WEBSITE IS SUBJECT TO AGREEING TO THIS DISCLAIMER
|
||||||||

Free to access Propofology Infograms, eBooks and selected YouTube videos by Dr. David Lyness are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Please attribute all works: 'Based on a work by Dr. David Lyness' at www.propofology.com/resources.
|
Home
About Contact |
ALL SITE USERS SHOULD READ AND AGREE TO THE DISCLAIMER HERE.
Contact via Twitter |



 RSS Feed
RSS Feed